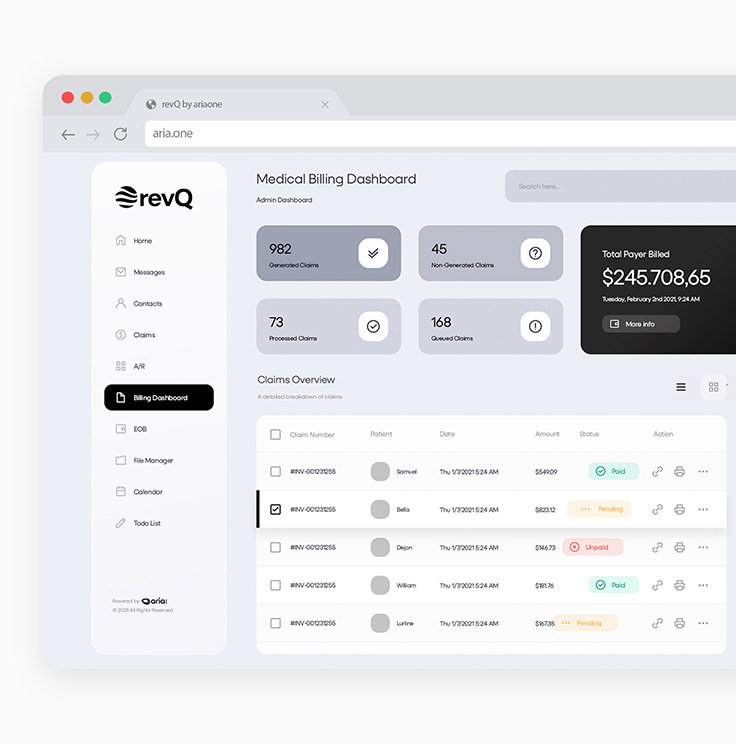
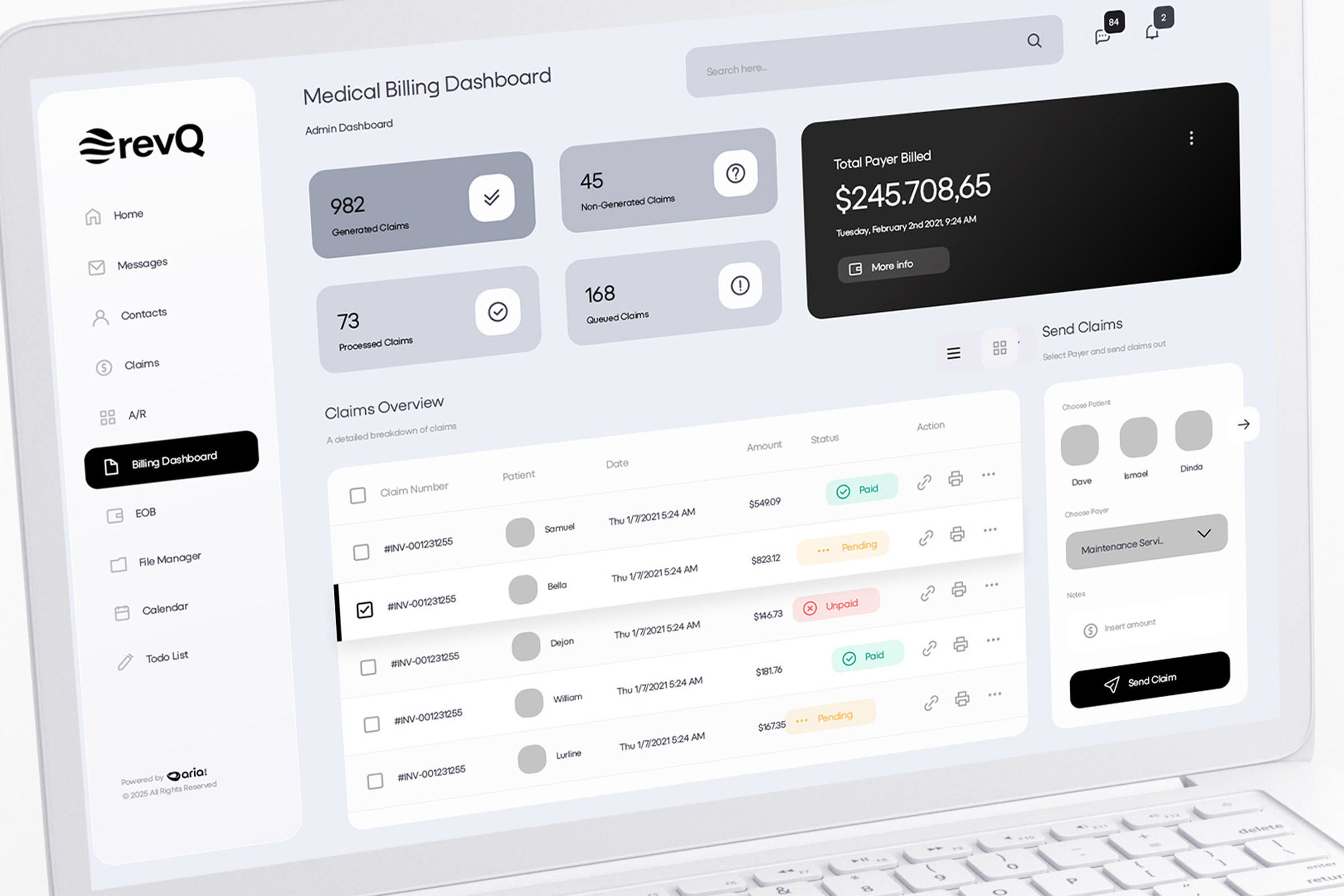
Cleaner claims. Faster cash.
RevQ automates and optimizes your revenue cycle from submission to reimbursement.
Introducing RevQ, the only billing solution you need. Eliminating the need for complex billing systems, replacing them with a simple method that stops losses before they happen.
Made for Revenue Teams, Not Just Billing Functions
Medical billing often fails when current systems are not able to adjust to new payer behavior, contract rules, or plan-specific policies.
RevQ was created to manage that complexity automatically. It accommodates payer, provider, and plan rules applying contract logic during payment and posting while prioritizing tasks based on financial value.
What Makes RevQ Different
Claims Do Not Move Forward Unless They’re Actually Ready
Many billing systems can sometimes let bad claims pass through. RevQ breaks that cycle. Before presenting claims, RevQ thoroughly validates them, checks for compliance, and applies correction rules. This will reduce preventable denials caused by simple mistakes.
Payments Are Interpreted And Processed Rather Than Posted Directly
Incoming payments are reviewed against contracts, coding, and billing principles to identify underpayments and missed revenue automatically.
Denials Are Decided, Not Just Worked
RevQ lets you categorize and manage denials to quickly see which are payable and which are not, helping you identify where effort is best spent.
What Makes RevQ Different
Built to Grow With Complexity
To improve future performance, RevQ continuously updates its guidelines and decisions by learning from outcomes such as approvals, denials, payments, and adjustments.
As payer behavior changes, RevQ changes with it.
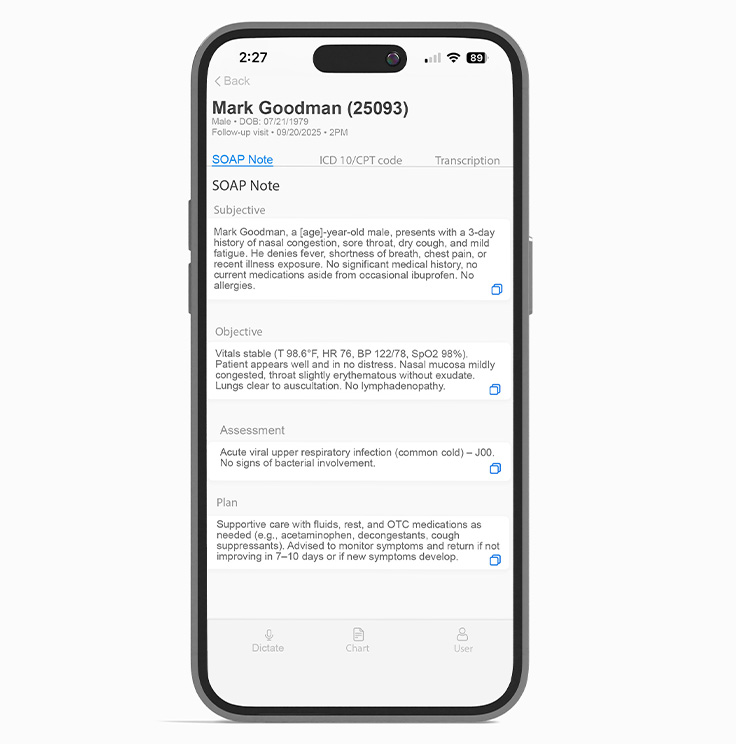
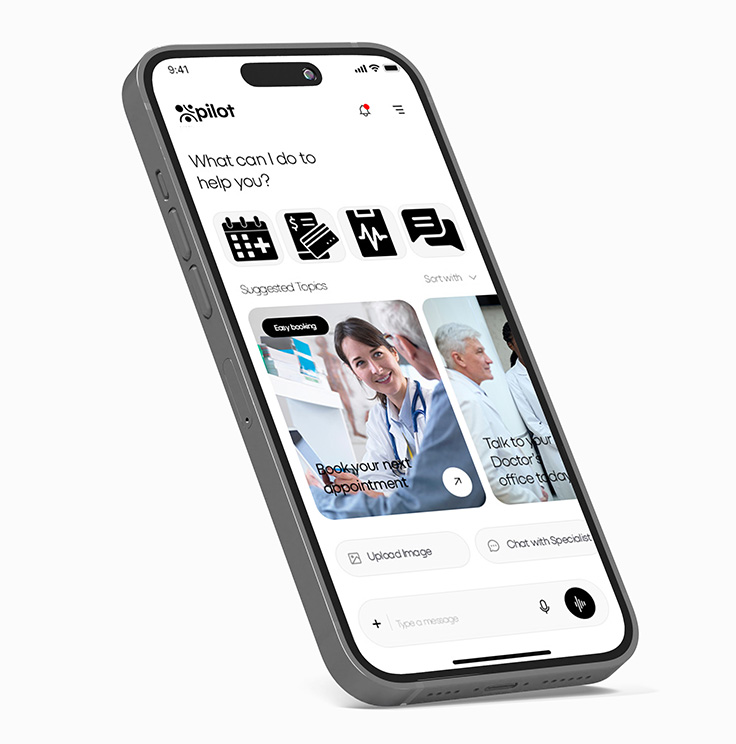
Part of the AriaOne AI Ecosystem
Lumina connects seamlessly with:
Our Impact
- Higher clean claim rates
- Short payment cycles
- Smaller denial backlog
- Fewer manual interventions
- Clear visibility into revenue risk and opportunity